When you have diabetes, Diabetic Wound Care Treatment for cuts, burns, abrasions, and basic wounds are a part of everyday living. But with diabetes it’s more important when it comes to healing. More often than not, we experience some form of injury or mishap, I mean no one has the invincibility of Superman or the immunity of Wonder woman! However, the case isn’t as straightforward with diabetics. These basic wounds and injuries, which many people class as insignificant or “it’ll go on its own”, have a more dramatic effect on the overall health of diabetics.
How to Treat Your Wounds

Diabetics often suffer enigmatic complications from very insignificant wounds; complications which, if not managed properly, can often be a threat to their very lives. So what are the ways in which diabetics can properly treat wounds? What information do diabetics require to arm themselves with the appropriate knowledge on how to treat even the most advanced wound complications? Well, we’re here to find out.
Understanding Just How Diabetes Works
Diabetes Mellitus, commonly known as Diabetes is a disorder of metabolism. To put this simply, a metabolic disorder is essentially a disorder that disrupts the natural process of metabolism (conversion and utilization of energy by organs of the body). In the case of diabetes, the focal zone is glucose (blood sugar) regulation.
INSULIN is a hormone, produced in the pancreas (an organ behind the stomach), that regulates the blood sugar in the body. Essentially, insulin is needed to move the sugar or glucose (converted from the breakdown of the carbohydrates we eat) around the body and into our cells. Our cells then store the glucose and provide the energy we need to carry out daily activities. Insulin disruption leads to the diabetic condition, and there are three main forms:
- Type 1 diabetes; which occurs when the pancreas is not producing enough insulin. People with type 1 diabetes need daily insulin injections to live.
- Type 2 diabetes; which occurs when the fat, liver, and muscle cells do not respond correctly to the insulin produced in the pancreas. Consequently, blood sugar does not get into these cells and can’t be stored for energy. This is the more diagnosed type of diabetes.
- Gestational Diabetes; which develops during pregnancy. In this form of diabetes, pregnant women without a prior history of diabetes, develop unusually high blood sugar levels. In gestational diabetes, blood sugar levels usually stabilize after delivery, but there is still the possibility of developing type 2 diabetes.

Diabetes may lead to many complications ranging from kidney damage, eye damage, cardiovascular disease, nerve damage, foot damage, skin conditions and healing impairment. Diabetes, unfortunately, has no cure (YET) and it is always advised to consistently manage, monitor and control blood sugar levels by eating healthily, exercising regularly and scheduling frequent health checkups.
How Does Diabetes Affect Healing?
As the title of this article suggests, we have sought out on a journey to understand the effective ways of treating diabetic wounds. But how exactly does diabetes affect healing?
The first and most important factor is blood sugar level. High blood sugar levels have the unwanted consequence of disrupting the body systems. When there is an accumulation of sugar (glucose) in the blood, the blood vessels begin to narrow and the arteries begin to stiffen.
As a result, blood is not circulated around the wound site making it difficult for oxygen to reach the wound and instigate healing. Also, increased glucose levels greatly decrease the functioning of red blood cells carrying nutrients to the injured area and consequently limit the ability of the white blood cells to fight infection.

Another very important factor that impairs the healing of wounds is diabetic neuropathy. Diabetic neuropathy is a type of nerve damage that can occur if you have diabetes. Elevated blood sugar levels often damage nerves throughout the body. This damage, in many cases, is irreversible and leads to an increasing numbness (loss of pain sensation) in the affected areas.
As a result, most patients do not feel sensation in their limbs, making it difficult to sense a blister, infection, or existing wound change and hence, utterly paralyze their abilities to heal. Diabetic neuropathy most often affects the nerves of the feet and legs, causing foot ulcers and leg wounds which heal slowly or hardly heal at all.
It is important to establish that high glucose levels also lower the body’s ability to fight infections by attacking and damaging the body’s immune system. This is called Immunosupression. In a high glucose environment, the immune system fails to efficiently produce the hormones associated with healing and thus, increases the risk of bacterial infections.
These bacterial infections have the ability to completely shut down the immune system and consequently, retard healing and increase the risk of infection. You don’t want infection setting in!
On to Diabetic Wounds
Now that we’ve understood the mechanism of infection and how diabetes impairs healing, we can proceed to understand how diabetic wounds can affect the health of diabetics.
As we’ve already established, Diabetic wounds are quite simply that: Wounds that are associated with diabetes. These wounds could be as insignificant as an insect bite, or as chronic as foot ulcers.
Many a time, the mechanisms of diabetes that impair healing are so significant that amputations may be necessary to avoid spread (if a wound is left untreated, it may become infected and spread locally to the muscle and bone [osteomyelitis] or to the blood stream [sepsis]) or death.
Diabetic wounds can occur on virtually every part of the body. However, one of the most prevalent forms of diabetic wounds is diabetic foot ulcers. I check my feet everyday without fail!
A diabetic foot ulcer is an open sore or wound which is sustained and complicated over a period of time due to high glucose levels causing a combination of neuropathic, weak immune system and poor circulation factors.
Diabetic foot ulcers affect around 15-20% of people with diabetes and according to a paper published in June 2017 in The New England Journal of Medicine, it is estimated that between 19% and 34% of diabetics will struggle with at least one foot ulcer in their lifetime, with about 20% of them requiring a total amputation.
Foot ulcers can transform from a tiny opening in the foot to a full-grown infection requiring amputation. The devastating part of this is: The transformation can literally happen overnight! It is CRUCIAL to examine your feet thoroughly on a daily basis!
Management and Treatment of Diabetic Wounds
Through a combination of diabetes-induced factors, diabetic wounds often have a hard time healing and can cause serious health complications. Diabetic wound management and treatment is of vital importance when dealing with diabetic wounds to ensure that the affected diabetic patient sustains an acceptable quality of life.
There are a number of steps to take when it comes to the treatment of a diabetic wounds. The first step to take is basic assessment of the wound. Diabetics who notice the onset of a diabetic wound are advised to see a doctor immediately. A diabetic wound could be classed as Ischaemic, Neuroischaemic or Neuropathic.
Upon examination, a medical professional (podiatrist) will identify which class the wound belongs to and proffer a viable treatment procedure. A failure to class a diabetic wound can lead to inappropriate wound treatment which may further complicate matters or possibly result in amputations.
The next step to take in the treatment of a diabetic wound (in this case a foot ulcer), is Wound Debridement. Debridement is the removal of dead or necrotic tissue from the wound area. This helps the medical professional to more closely examine the underlying area, provide drainage for the wound, and optimize the effectiveness of the wound dressing.
After necrotic tissue has been removed and adequately dressed, the next step to take is Infection Control. Exposed diabetic wounds are prone to infections and complications, hence it is important to ensure that they are guarded as sensitively as possible. Topical antibiotics, Anti-bacterial ointments and lotions and Topical antimicrobials should be appropriately applied to reduce the possibility of further complication from infections.
Also, advanced wound care dressings (such as Honey sheet dressings, Alginate dressings, and Occlusive dressings, amongst others) help to balance moisture and give the wound a chance to drain and heal properly.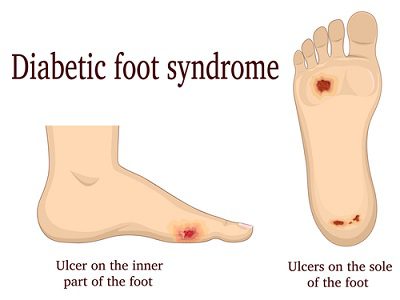
In the case of Foot or leg ulcers, an important treatment to consider is Pressure Offloading. Medical professionals have proved that taking pressure or weight off a wound can greatly reduce the likelihood of complications by giving the affected area more room to breathe and thus, fractionally improving healing.
In the more extreme cases of diabetic wounds, surgery may be required to alleviate the possibility of long-term complications to the diabetic’s health. Amputation is the ultimate necessity when a wound has been complicated to the point of no return.
The Role of Nutrition in Diabetic Wound Treatment
Diabetic wounds are complicated by a variety of factors, chief among them being elevated blood glucose levels. The importance of nutrition to stabilizing these high blood sugar levels cannot be under-emphasized. Poor nutrition can result in altered immune function and poor glycemic control which are risk factors for poor healing.
As a result, the National Pressure Ulcer Advisory Panel (NPUAP) has established evidence-based nutrition recommendations for the prevention and treatment of pressure ulcers. These nutritional recommendations help to ensure that blood sugar levels are regulated whilst promoting immune system functions for the overall health.
Conclusion
Diabetic Wound Care Treatment is important and more so when you have diabetes than not. Statistics show that by 2030, around 600 million people around the world would be diabetic, with approximately 30% developing some form of diabetic wound or the other during their lifetime (20% of these being foot ulcers). Diabetic wound treatment is critical to address as soon as possible.
It is important to identify and prevent the onset of diabetic wounds and manage them effectively once they appear in order to greatly improve quality of life and ensure a prolonged existence irrespective of the odds.
Check Out Below the Best Way
to Lower Your Blood Sugar Fast!
Please share on social media below and forward this to others who need help and please leave any questions or comments you may have below. I would love to interact with you. Thank you for reading and I appreciate it!
- Amazon Kindle Edition
- Rothchild, Sascha (Author)
- English (Publication Language)
- 336 Pages - 04/19/2022 (Publication Date) - G.P. Putnam's Sons (Publisher)
- ✅ QUICK AND EASY TO USE: Care Touch blood sugar test kit delivers results in only 5 seconds with just a 0.5µL blood sample. There is no programming needed since our blood sugar monitor kit automatically recognizes batch codes encrypted on Care Touch glucose test strips. Our state-of-the-art glucometer kit with strips and lancets includes single-touch strip ejection, so you can hygienically remove used diabetic test strips.
- ✅ EASY DIABETIC MONITORING: The blood sugar monitor kit with strips is capable of saving up to 300 readings. The blood glucose test kit also provides a continuous 14-day average of your readings, making glucose monitoring easy for you and your healthcare provider.
- ✅ PORTABLE AND HASSLE-FREE: The diabetic testing kit comes with a handy glucometer case, which means you can check your blood sugar level at home or anywhere else while staying organized. The 10-depth lancing device and lancets will help make blood sugar testing almost painless and hassle-free.
- ✅ COMPLETE DIABETIC SET: The glucose meter kit with strips and lancets includes: (1) Care Touch Blood Sugar Meter, (100) Blood Glucose Test Strips for diabetes, (1) Lancing Device, (100) Lancets for diabetes testing, (1) 3 Volt Lithium Battery, (1) Glucose meter case for your blood sugar tester and diabetic supplies
- ✅ WE CARE BECAUSE YOU CARE: You care about your health, and we care about you. Care Touch is committed to providing the best quality blood glucose monitoring systems. Our care doesn’t end when your sugar tester diabetes kit arrives at your door. We’re fully dedicated to your satisfaction. If you have any questions or concerns about your glucose monitor kit with strips and lancets - contact us at any time.
- Amazon Prime Video (Video on Demand)
- English (Playback Language)
- English (Subtitle)
- PUREHEALTH RESEARCH - Blood Sugar Formula 3 Bottles
- MANUFACTURED in the USA! 365-DAY SATISFACTION GUARANTEED!
- A DOCTOR-APPROVED NATURAL FORMULA. Seventeen potent ingredients, each scientifically proven to have a significant effect at helping balance your glucose levels, improve glucose sensitivity, protect delicate cells from free radicals, and energy
- HIGH POTENCY. PureHealth Research experts scientifically enhance CHROMIUM with the Vitamin C, E, Mulberry Leaf, Bitter Melon, Cinnamon, L-Taurine, Berberin and other ingredients which are proven to help you support healthy blood glucose levels
- ONE CAPSULE DAILY, THREE BENEFITS: supports healthy sugar and carb absorption, supports insulin levels, supports cardiovascular health
- Scientifically formulated; great care was put into combining just the right amount of 20 different ingredients into a premium formula designed to support healthy blood sugar levels
- High potency support for 365 days a year; the unique combination in this blend is crafted to help support healthy glucose absorption and glucose production by your body; contains Gymnema, Alpha Lipoic Acid, Yarrow, Licorice, Cayenne, Banaba, Guggul, Bitter Melon, Juniper Berry, White Mulberry, L-Taurine & more
- One capsule twice a day, five benefits; (1) supports normal blood sugar levels; (2) supports weight control and energy; (3) supports healthy sugar and carb absorption; (4) supports insulin levels; (5) supports heart health; daily support for healthy blood glucose levels, 365 days a year
- Reliable; made in a GMP certified facility in America and third party safety tested for purity
- Great value for money; 120 vegetarian capsules for a 60 days supply
Last update on 2022-06-23 / Affiliate links / Images from Amazon Product Advertising API








I am actually a fairly new diagnosed Type II diabetic and I am an Emergency Medical Technician. I have seen many wounds that were exacerbated by the patient having diabetes. It’s crazy how that disease can make even the simplest injury on the feet difficult to heal. Thanks for writing this article about diabetic wound treatment.
Are you also a diabetic? Or is this just a subject of interest for you?
Hey Brian 🙂
Sorry to hear that you were diagnosed with this disease.
But knowledge is power and we can control it.
As you mentioned, I’m sure you’ve seen many wounds and then some. And of course it’s worse with diabetes.
I check my feet everyday because I am type 2 diabetic. This subject is just one of hundreds I talk about on my website.
Thank you for commenting and for your service in your field! 🙂
HI Rob, My father suffered from diabetes for much of his adult life – 80% of Australians who pass away from natural causes do not with some version of diabetes – many without even knowing it. From my dad though I can fully attest to the difficulties that diabetes sufferers go through when they cut themselves. My father did not have to inject, however he did have to monitor daily. And the same clotting features you mention to do with lack of oxygenated blood to the wound site also caused other complications and a minor stroke. Which then led to drugs to thin his blood.
So when dad cut himself, which he did often as he loved to work in his garden, he had to deal with circulation issues you mentioned which led to infections and ulcers. then once he had his stroke and was on blood thinners, his biggest problem was then losing too much blood as it didn’t clot – which then also led to a reduction in blood sugar levels and so the merry-go-round started again.
Your site is a lifesaver as I am a firm believer in anything that raises community knowledge about diabetes and how to manage it. My dad often mentioned that he wish he had found out about his earlier in life – or at the very least been able to better manage diet etc. Keep up the good work.
Paul
Hey Paul,
I’m very sorry to hear about your dad. Diabetes is such a difficult thing to live with.
Cutting yourself is extremely hard because you have to be careful as you mentioned.
Ulcers and infections can be very serious as you already know.
It’s crucial to check and keep your blood sugars in the normal range to avoid this issues.
I want to help every person with diabetes with controlling it because I know how serious it is and how important it is to keep in under control.
Thank you so much for sharing! 🙂
Hi Rob!Your website is a very nice website.You have elaborated and explained all the requirements on how to treat diabetes.This website will be of great help to many people to find the right ways for diabetes treatment.Though I am not a diabetic patient, I would surely recommend this website to others with diabetes and issues with wounds especially.I hope your website will be of great help to many people!
Cheers
Ramesh
Hi Ramesh 🙂
Thank you for saying. It’s my goal to help others with diabetes.
I’d like to spread the word about the natural ways to lower blood sugar and to avoid getting any wounds because that is serious with diabetes.
While diabetes can cause many problems, I wanted to point out the dangers of getting any wounds with diabetes.
Having your feet checked daily is a very necessary task to say the least.
Anyone with diabetes must be extremely careful with receiving any wounds and get immediate treatment.
I appreciate your thoughts! 🙂